- internistic

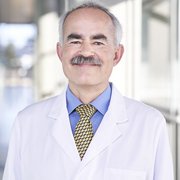
Prof. Dr. med. Thomas Seufferlein
Ärztlicher Direktor der Klinik für Innere Medizin I (Speiseröhre, Magen, Darm, Leber und Niere sowie Stoffwechselerkrankungen) und Sprecher des Darmzentrums

Dr. med. Thomas J. Ettrich
Oberarzt, Leiter Schwerpunkt GI-Onkologie, Leiter des klinischen Studienzentrums GI-Onkologie
Schwerpunkte
Gastrointestinale Onkologie, Klinische Studien

Dr. med. Angelika Kestler
Funktionsoberärztin, Fachärztin für Innere Medizin und Gastroenterologie, Palliativmedizin, Ärztliche Referentin für GI-Onkologie am CCCU
Schwerpunkte
Gastrointestinale Onkologie, Privatambulanz Prof. Seufferlein
- Surgical

Prof. Dr. med. Marko Kornmann
Stellv. Ärztlicher Direktor/ Koordinator Viszeral-Onkologisches Zentrum
Schwerpunkte
Bereichsleitung Bauchspeicheldrüsen-, Magen- und Speiseröhrenchirurgie

Prof. Dr. med. Emrullah Birgin
Schwerpunkte
Bereichsleitung Leber- und Gallenwegechirurgie
Ärztliche Leitung Studienzentrum
Description of the disease
Hepatocellular carcinoma is the term used to describe cancer arising from liver cells (so-called hepatocytes).
Frequency and age of onset
Primary liver cancer is a rare disease in Europe; secondary liver tumours, such as liver metastases from other cancers, are much more common in the liver. In Germany, an average of 5 people per 100,000 inhabitants are diagnosed each year, with men being affected three times as often as women. The peak age is between 60 and 70 years.
Causes and risk factors
The main cause of liver cancer is liver cirrhosis, i.e. the final stage of chronic liver disease. Patients with liver cirrhosis due to chronic hepatitis B infection or hepatitis C infection and patients with liver cirrhosis due to chronic harmful use of alcohol or other liver diseases have the highest risk of developing liver cancer.
Signs of illness
There are no characteristic signs of liver cancer. They may include pressure pain in the right upper abdomen, weight loss, abdominal fluid formation, a worsening of pre-existing liver cirrhosis and fever.
Diagnostik, Therapie, Prognose
Weitere Informationen zu Diagnostik, Therapie, Prognose siehe: www.krebsinformationsdienst.de/leberkrebs
Blauer Ratgeber der Deutschen Krebshilfe: www.krebshilfe.de/die-blauen-ratgeber