Focus on lipodystrophies and fatty tissue diseases

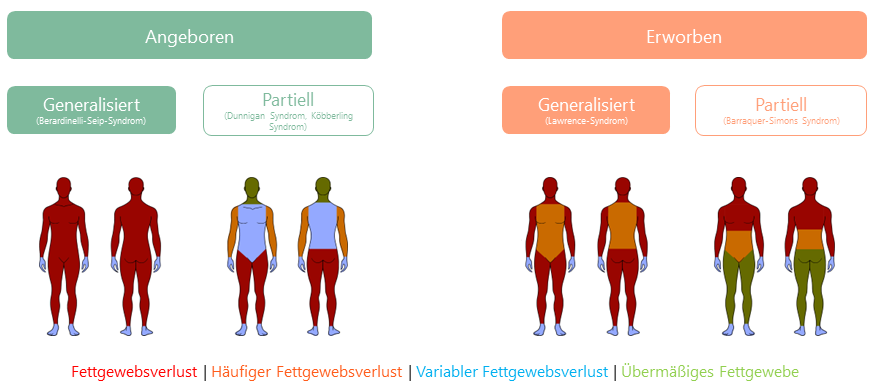
Lipodystrophies are very rare diseases characterised by a lack of subcutaneous fatty tissue or a maldistribution of subcutaneous fatty tissue and the resulting metabolic changes. Lipodystrophy diseases can be classified according to their aetiology (genetic or acquired) and the extent and extent of the loss of fatty tissue (generalised or partial).
In generalised lipodystrophies, the loss of subcutaneous fatty tissue affects the entire body, whereas in partial forms only parts of the body are affected. There are four main categories: congenital generalised lipodystrophy (CGL), familial partial lipodystrophy (FPL), acquired generalised lipodystrophy (AGL) and acquired partial lipodystrophy (APL).
Some causative genetic changes (mutations) have already been identified for the congenital forms. However, the cause of a large proportion of genetic lipodystrophies is still unknown. Acquired lipodystrophy can have various causes, such as immunological disorders, infections or the administration of certain drugs, in particular antiretroviral drugs as part of HIV therapy or insulin.
Due to their rarity and their great clinical heterogeneity and correspondingly variable symptoms, lipodystrophies are difficult to diagnose and are often only recognised very late. Lipodystrophies can be diagnosed by precisely analysing the clinical phenotype and, if necessary, by genetic testing. For a large proportion of patients, regular annual examinations for secondary diseases are recommended.
Lipodystrophies are often associated with hormonal and metabolic changes that can lead to severe metabolic complications. These depend on the subtype of lipodystrophy, the extent of adipose tissue loss, age and gender. Due to the lack of adipose tissue, patients often suffer from a deficiency of the hormoneleptin. Leptin is produced in adipose tissue and plays a central role in energy homeostasis as well as fat and glucose metabolism. Leptin deficiency leads to metabolic and hormonal disorders, loss of fat under the skin and fat accumulation in the liver (up to fatty liver), in the muscles and in the blood (hypertriglyceridaemia). Furthermore, insulin resistance can occur with increased blood glucose levels, which can result in diabetes mellitus that is difficult to treat. The regulation of satiety can be disturbed, which can lead to hyperphagia (increased food intake due to a lack of satiety) and thus increased calorie intake. Excess fatty acids are deposited in other organs such as the liver, kidneys and muscles due to the lack of adipose tissue, which leads to tissue damage.
Leptin also plays an important role in the immune system and sexual maturity. This can therefore lead to increased infections and disruptions in pubertal development and fertility. Particularly in patients with generalised lipodystrophy, leptin levels are very low, which leads to a particularly severe manifestation of secondary diseases and a considerable impairment of the quality of life of those affected.
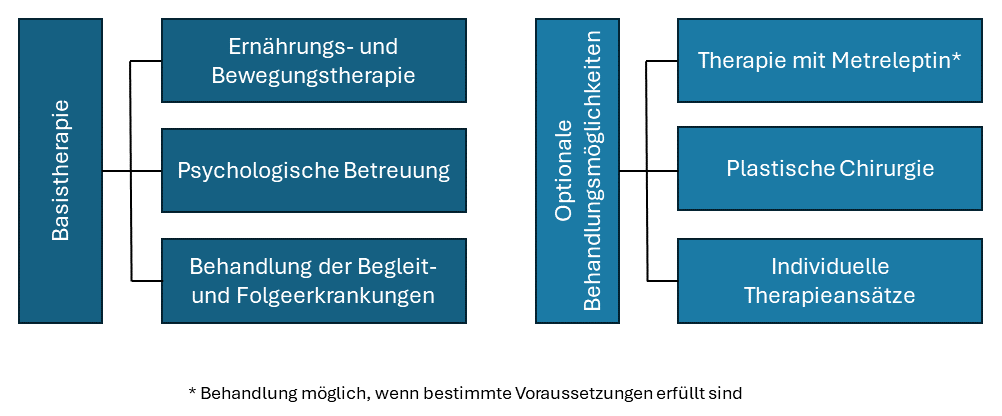
There is currently no cure for lipodystrophy. Specialised nutritional therapy is essential for the treatment of the metabolic consequences. Patients with certain forms of lipodystrophy and low leptin levels may benefit from specialised therapy. Metreleptin, a recombinant human leptin analogue, is used as a leptin replacement therapy in combination with a diet to treat the consequences of leptin deficiency. The leptin supplied increases the breakdown of fat in the blood, muscles and liver and thus leads to a dramatic improvement in hypertriglyceridaemia, fatty liver, insulin resistance and diabetes mellitus. However, the lost subcutaneous fat tissue cannot be restored by leptin replacement therapy.
Other non-specific therapeutic approaches can also help to treat the secondary diseases of lipodystrophy (e.g. metformin for diabetes, statins or fibrates for hyperlipidaemia).
Consultation hours
University outpatient clinic for lipodystrophies and fatty tissue diseases(during our consultation hours)
Specialised care within the framework of the ZSEE
Patients with lipodystrophies are treated at Ulm University Hospital under the umbrella of the Centre for Rare Diseases (ZSE) in the Specialist Centre for Rare Endocrine Diseases (ZSEE) by selected experts. We carry out leptin replacement therapy with the active substance metreleptin (trade name: Myalepta) at our centre. The treatment should be initiated and monitored by experts who have experience in the diagnosis and treatment of metabolic disorders. Patients will receive comprehensive training on the use of the drug from their doctor or healthcare professional. Further information on Myalepta can be found at www.myaleptainfo.eu.
Contact person

Prof. Dr. med. Martin Wabitsch
Leiter Sektion Pädiatrische Endokrinologie und Diabetologie
Schwerpunkte
Endokrinologie und Diabetologie
Ernährungsmedizin
Fachbezogene genetische Beratung
Experimentelle Endokrinologie


Dr. med. Roza Sabia
Funktionsoberärztin Sektion Endokrinologie, Fachärztin für Innere Medizin, Endokrinologie und Diabetologie, Zusatzbezeichnung Ernährungsmedizin
Schwerpunkte
Endokrinologie

Gisa Ufer
Fachärztin für Innere Medizin, Fachärztin für Endokrinologie und Diabetologie, Zusatzbezeichnung Ernährungsmedizin
Lipodystrophy round table
Are you affected by lipodystrophy and have questions on specific topics? Would you like to exchange ideas with other sufferers?
The Lipodystrophy Stammtisch was set up jointly by the German Lipodystrophy Reference Network and the NetLip patient network. Every first Tuesday of the month, the Stammtisch invites you to get to know and exchange ideas with other sufferers. The regulars' table takes place online. You can obtain the access data from the NetLip patient network (netlip@netlip.org).
Experts on a specific topic are also invited at regular intervals. The experts give a short presentation and then answer all your questions.
We look forward to seeing you!
Next dates:
03.12.2024; 7:30 pm
07.01.2025; 7:30 pm
04.02.2025; 7:30 pm
Save the Date: Lipodystrophie Patiententag 2026!
Der Termin für den Lipodystrophie Patiententag 2026 steht fest: 18.04.2026.
Er wird nächstes Jahr in Ulm stattfinden und in Zusammenarbeit mit dem Patientennetzwerk NetLip und dem Deutschen Referenznetzwerk Lipodystrophie (Uniklinik Leipzig und Ulm) veranstaltet. Details zum Programm und zur Organisation folgen zu einem späteren Zeitpunkt.
Wir freuen uns auf Ihr Kommen!