Welcome to the website of the Section for Interdisciplinary Pancreatology, or SIP for short.
The SIP was founded in September 2022 and offers you, dear patients, highly specialised, maximum visceral medical care for diseases of the pancreas (pancreatology) according to the latest scientific standards.
At the SIP, we offer you the entire range of services of pancreatological university visceral medicine. Visceral medicine treats patients with diseases of the abdominal and digestive organs, which often require perfect interaction between gastroenterology and general and visceral surgery for optimal treatment success.
This interaction has already been anchored in the organisational structure of the SIP as a novelty, whereby the visceral medical idea is predetermined with a management structure based on parity:
The internal medicine and pancreatology side is managed here by Prof. Alexander Kleger (Section Head of SIP and Director of the Institute of Molecular Oncology and Stem Cell Biology) and the surgical, pancreatological side is represented by Prof. Dr Marko Kornmann (Deputy Section Head of SIP and Deputy Medical Director of Visceral Surgery).
This means that you, dear patients, can be optimally examined and treated on an interdisciplinary basis without delay during your outpatient appointment or inpatient stay. In this way, we specifically try to bundle repeated appointments and have defined all diagnostics and therapies for you in advance in accordance with the latest standards and guidelines adapted to the development of medical science in corresponding treatment paths. The majority of patient-specific decisions in the SIP are made within the framework of so-called board structures analogous to the classic tumour board after detailed review and discussion of all findings and demonstration of the corresponding imaging material (e.g. computer tomography, endosonography or magnetic resonance imaging). There is close cooperation with our CCCU (Comprehensive Cancer Centre Ulm). This brings together various medical disciplines, including gastroenterologists, visceral surgeons, radiologists and, if necessary, pathologists, in order to offer you, our patients, the best possible interdisciplinary treatment tailored to your needs.
Pancreatological University Medicine reflects the interface between patient care and research. In line with this mission statement, we also work on various scientific issues and collect biomaterial (e.g. blood or urine samples, organoids), use questionnaires to record your personal well-being during and after the clarification of your individual illness, all in order to further improve the treatment and prognosis of patients with pancreatic diseases and their satisfaction in the long term. Here, too, co-operation with you and all professional groups involved is particularly important to us.
We would like to take this opportunity to thank you for your trust and look forward to supporting you as best we can with your illness.
Yours
Alexander Kleger and Marko Kornmann

Management

Prof. Dr. rer. med. Alexander Kleger
Leiter Sektion Interdisziplinäre Pankreatologie, Direktor Institut für Molekulare Onkologie und Stammzellbiologie, Heisenberg Professor für Molekulare Onkologie, Leiter Core Facility Organoids
Schwerpunkte
Erkrankungen der Bauchspeicheldrüse
Team members

Prof. Dr. Marko Kornmann
Stellv. Sektionsleiter SIP, Stellv. Ärztlicher Direktor Allgemein- und Viszeralchirurgie, Koordinator Darmzentrum


With which illness should you present at the SIP?
At the SIP, we mainly look after patients with all forms of precancerous conditions such as pancreatic cysts or benign tumours, malformations and acute and chronic pancreatitis. We also offer university screening programmes for patients who have an increased risk of developing pancreatic cancer due to genetic diseases (pancreatic tumour predisposition syndromes). We offer a wide range of surgical and non-surgical treatments using modern and innovative technical instruments. Diagnostics are mainly based on imaging procedures but also punctures, which are then carried out as part of an inpatient stay if necessary. In particular, we also use endoscopic procedures such as endosonography (ultrasound examination performed from the inside) or ERCP(endoscopicretrogradecholangiopancreatography; here, the bile ducts, the gallbladder and the pancreatic duct are visualised with the help of X-ray contrast medium and a special endoscope). These examinations are mapped using interventional endoscopy. High-resolution MRCP(magnetic resonancecholangiopancreatography) also plays an important role. It is an examination of the bile ducts and the pancreatic duct using magnetic resonance imaging (MRI). Further details and information material can be found in the explanation of the respective clinical pictures on our homepage. The following diagram illustrates the clinical pictures of SIP:
What is the advantage of interdisciplinary care for patients with pancreatic diseases?

The key word here is symbiosis - mutual complementation and support through collaboration between different disciplines.
In line with the university's medical mission statement - patient care, research and teaching - we work together with the entire Department of Internal Medicine 1, the Department of Visceral Surgery and, of course, with research institutions such as the Institute of Molecular Oncology and Stem Cell Biology, which enables us to review and apply findings from research.
The problems of pancreatological patients require interdisciplinary cooperation
Patients with chronic pancreatitis in particular develop different problems in different phases of the disease, which in turn require specific and customised treatment. At SIP, we provide the right therapy for each of these phases and naturally also try to influence the progression of the disease as far as possible.

Some facts:
Various cystic changes can develop in the pancreas. In addition to mucinous-cystic neoplasia (MCN) and intraductal papillary-mucinous neoplasia (IPMN), the group of cystic pancreatic lesions also includes serous-cystic neoplasia (SCN) and serous-pseudopapillary neoplasia (SPN). The term neoplasia refers to a benign or malignant neoplasm of body tissue caused by a dysregulation of cell growth.
These four clinical pictures mentioned above are among the most common cystic neoplasms of the pancreas and differ in terms of frequency, malignant potential and histology. Some of these lesions are associated with a higher incidence of pancreatic cancer. Precise diagnostics for the exact categorisation of the respective "cyst" is crucial for further therapy and an essential part of our work at the SIP.

Diagnostics and control
In addition to the classification of pancreatic cysts, regular, sometimes lifelong monitoring of the respective lesions is often necessary. To do this, we use state-of-the-art imaging techniques such as endoscopic ultrasound (endosonography, EUS) and magnetic resonance imaging (MRI). It is often necessary to take a sample from the pancreas, e.g. to examine the secretion within the cyst or to have the extracted cells examined for "irregularities" by an experienced pathologist. The aim of all these examinations is to be able to better assess the risk of degeneration of the respective cyst. It is particularly important to us that we discuss our decisions on an interdisciplinary basis. Together with an experienced abdominal surgeon (visceral surgeon) and an experienced radiologist, who will explain the images you have provided to us in detail, we will make a joint decision on further treatment. The findings will result in various risk categories, which we will use to determine whether the cystic neoplasm should be operated on or simply monitored regularly.

Therapy
Depending on the risk category, we may recommend that you have regular check-ups in our SIP outpatient clinic. We will plan the interval and the respective examinations (MRI, EUS) accordingly. If surgery is required, the most gentle procedure for you will be determined and discussed with you on an interdisciplinary basis. In Ulm, we have been continuously focussing on the development of minimally invasive solutions for several years and, where technically possible, we use the daVinci ecosystem, which provides the surgeon with an extensive additional portfolio alongside the classic robot-assisted surgical platform and enables the respective operation to be performed gently and safely with the best possible overview.
Acute pancreatitis (AP) is an acute, primarily sterile inflammation of the pancreas. Damage to the glandular tissue leads to an unphysiological activation of the digestive enzymes of the pancreas, which can result in an inflammatory reaction with oedema, vascular damage and possibly even cell death. The most common causes are increased alcohol consumption and gallstone disease. The course of this disease is very variable - from uncomplicated to life-threatening. In 2019, 92,449 cases ofpancreatitiswere diagnosed in hospitals in the Federal Republic of Germany (94,877 cases are forecast for 2021). In Germany, the incidence is between 13 and 43/100,000 inhabitants/year, with regional fluctuations being particularly noticeable. In comparison, the diagnosis of "heart attack" was made around 220,000 times in 2019. This means that AP is a relatively common disease with clinical relevance. The treatment of patients with a severe course of the disease is usually complicated and prolonged and should be carried out at a specialist centre. At the same time, there is often a transition to chronic pancreatitis. Therefore, prompt diagnosis and efficient treatment of AP are of particular importance. The treatment of AP has changed considerably over the past 10 years, with some of the concepts established a few years ago being completely reversed. At SIP, we ensure standardised interdisciplinary care in accordance with the latest research at all levels at all times.
Chronic pancreatitis (CP) is defined as a disease of the pancreas in which the pancreatic tissue is replaced by fibrotic connective tissue due to a persistent inflammatory reaction with recurrent inflammatory episodes. CP is a relatively common gastroenterological disease that is mostly treated on an outpatient basis. In the western world, the incidence of CP is approx. 5-12/100,000, the prevalence is approx. 50/100,000. The number of new cases varies greatly around the world, which can be attributed in particular to socio-cultural differences in alcohol consumption. As a result of fibrotic tissue remodelling, there is a progressive loss of organ function. The function of the pancreas is divided into so-called exocrine and endocrine function. The exocrine function consists of the provision of digestive enzymes; a lack of function ("insufficiency") leads to digestive problems such as diarrhoea, abdominal pain and flatulence and even malnutrition. The endocrine function consists primarily of the release of insulin and thus the regulation of blood sugar, an insufficiency ultimately means the development of diabetes mellitus. Furthermore, CP is a recognised risk factor for the development of pancreatic cancer. With a continuously increasing incidence and still poor prognosis, pancreatic carcinoma occupies a special position within gastrointestinal tumours. In everyday clinical practice, the detection of pancreatic carcinoma in patients with CP represents a major diagnostic challenge. A distinction must also be made between acquired and hereditary pancreatitis, as the latter carries a higher risk of developing pancreatic cancer, whereas the risk is only slightly higher in the case of pancreatitis caused by alcohol, for example. At the same time, this shows that patients with hereditary pancreatitis must be given special attention with regard to tumour prevention.
Some facts:
While the majority of pancreatic carcinomas (pancreatic cancer) occur sporadically, i.e. without a recognisable congenital predisposition, a congenital and often familial predisposition can be identified in some cases. Recognising these cases is important as they pose a significant risk of developing pancreatic cancer for both the patient and, where applicable, their relatives, and thus the need for targeted early detection measures. In addition, some of the syndromes are also associated with a risk of malignant tumours outside the pancreas.
These syndromes include
- Familial pancreatic carcinoma
- Forms of hereditary pancreatitis
- Tumour predisposition syndromes of several organs: Peutz-Jeghers syndrome, familial atypical multiple mole and melanoma syndrome (FAMMM), Li Fraumeni syndrome, hereditary breast and ovarian carcinoma (HBOC), Lynch syndrome, ataxia teleangiectasia
Familial pancreatic carcinoma is assumed if at least two first-degree relatives (siblings or direct descendants) have pancreatic carcinoma, but none of the other known risk syndromes are present. In addition to taking a family history of the disease, molecular genetic tests are available to identify known causative genetic changes.
Hereditary pancreatitis (hereditary pancreatitis) is usually triggered by changes in the PRSS1 gene, which lead to changes in pancreatic secretions. This disease is characterised above all by repeated episodes of acute pancreatitis at a young age, but is also associated with an increased risk of developing pancreatic cancer. Hereditary pancreatitis is a particular focus at SIP. We take care of all aspects of the disease. From diagnosis and monitoring to symptomatic, medicinal and invasive therapy. We work closely with Prof Jonas Rosendahl (University Hospital Halle) and the Ulm Institute of Human Genetics (Prof Reiner Siebert), particularly in the field of diagnostics.
Hereditary breast and ovarian cancer is usually caused by gene mutations in BRCA1 and BRCA2, less frequently by other mutations, for example in PALB2.
Peutz-Jeghers syndrome manifests itself, among other things, with numerous benign polyps in the gastrointestinal tract and is associated with an increased risk of pancreatic cancer.
Familial atypical multiple moles and melanoma syndrome (FAMMM) is usually first discovered through many so-called atypical naevi (moles) and the development of melanomas (black skin cancer). However, the risk of ever developing pancreatic cancer is increased by around 20%.
Li-Fraueni syndrome, Lynch syndrome and ataxia telangiectasia are also associated with an increased risk of developing pancreatic cancer.
Early detection tests: If a significantly increased risk of developing pancreatic cancer is identified, early detection measures can be considered. These include endoscopic ultrasound and magnetic resonance imaging.
In endosonography, an ultrasound probe is placed in the gastrointestinal tract in the immediate vicinity of the pancreas as part of an endoscopy, similar to a gastroscopy, and can thus produce high-resolution images of the gland.
In magnetic resonance imaging, images of the pancreas are produced in a strongly magnetic tube without the use of radiation.
If tumours or precursors with a high risk of degeneration are detected, a team of internists, radiologists and surgeons will discuss the best treatment recommendation for the individual patient. The SIP offers a dedicated screening programme in accordance with international guidelines.
Research:
At SIP, we are particularly proud of our function as a translational interface for basic research. A particular focus is on research into the development of familial pancreatic carcinoma (FPC), hereditary pancreatitis and monogenetic diabetes in the context of germline mutations. We generate human pluripotent stem cells from the hair roots of affected patients and use these for functional analyses. This enables us to bring basic research directly into the clinic and answer relevant scientific questions.

Some facts:
During the development of a human being from the fertilised egg, the pancreas is initially created in two buds in the area of the future small intestine, one anterior (ventral) and one posterior (dorsal). These two buds usually fuse to form one organ. While in most cases the organ is therefore located on one side of the duodenum and the secretions from both systems drain into the intestine via a common duct, around 1 in 10 people have a different anatomy. This usually has no pathological value, but can lead to symptoms and complications in some cases. The most common anomalies are
- The pancreas divisum
- The pancreas anulare
- Ectopic pancreatic tissue
In pancreas divisum, the two pancreatic anlagen do not fuse completely into one unit and, in particular, the outflow of secretions remains completely or partially separate. As a result, the majority of the organ does not release its secretions into the intestine via the large common duct, but via a relatively thin duct. Whilst this does not cause any problems for most people, some people suffer from recurrent abdominal pain and episodes of acute pancreatitis, presumably due to a build-up of secretions. Patients with few symptoms benefit from a dietary adjustment. However, if pancreatitis occurs, endoscopic dilatation of the duct system, which is too small, may be necessary.
With pancreas anulare, a ring of pancreatic tissue remains around the duodenum as the anterior and posterior anlage move towards each other around the duodenum. This can lead to an intestinal obstruction in early childhood due to constriction of the duodenum. However, it is also possible that symptoms only manifest at an advanced age. Treatment is usually surgical.
In the case of ectopic pancreatic tissue, normal pancreatic tissue lies outside the actual gland, which generally causes no symptoms, but in some cases can lead to pain due to inflammatory processes.
At the SIP, we take care of diagnostics as well as the appropriate treatment. Here too, interventional decisions are made on an interdisciplinary basis in order to provide you with the best possible treatment.



Contact & Appointments
Consultation hours:
Monday: 13:00 to 17:00
Pancreas phone:
0731/500-44732
Directions/Arrival:
Medical Clinic
Lift area A, level 1
Albert-Einstein-Allee 23
89081 Ulm
Well signposted from the main entrance -> Outpatient Department of Internal Medicine
Further medical training in IgG4-associated diseases on 11.12.2024
We are pleased to inform you that we will be holding a medical training course on the topic of IgG4-associated diseases on 11 December 2024.
During an evening of lectures, you will have the opportunity to refresh your knowledge of this rare disease entity, ask us questions and get to know us over dinner.
Details and registration for the event can be found in the following document.
We look forward to seeing you.
SIP approved as a study centre for the INDIGO study
As one of the first German study centres, our section has now been approved for the INDIGO study, in which a new drug for IgG4-associated disease is being tested.
You can find a detailed report under the following link:
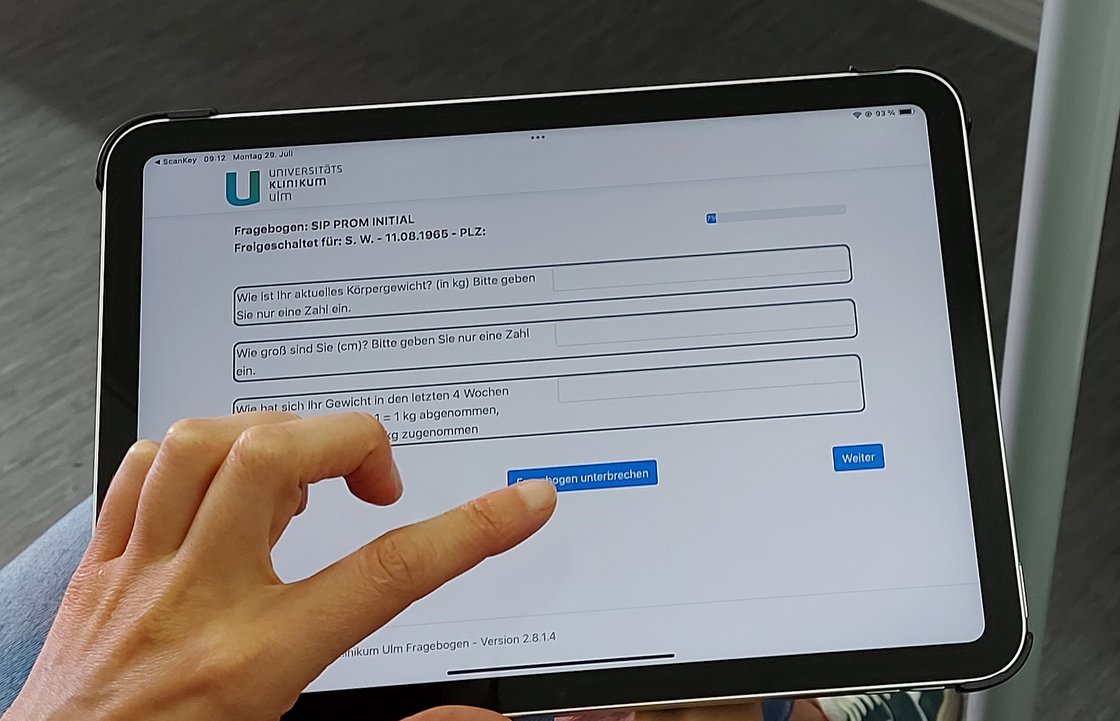
Digitised patient questionnaires in the pancreas outpatient clinic
Since the beginning of the year, we have been able to hand out digitised patient questionnaires to patients in our outpatient clinic using iPads.
This allows us to systematically collect disease-relevant findings and we hope that this will enable us to optimise patient care in the future and better characterise our patient population.
German Cancer Prize 2023 for Prof Alexander Kleger

Prof Dr Alexander Kleger has been awarded the German Cancer Prize 2023 in the "Experimental Research" category for his pioneering and innovative research approaches in cancer medicine.
The German Cancer Prize is one of the highest honours in oncology and is awarded annually in the categories "Clinical Research", "Translational Research" and "Experimental Research" for outstanding work in German-speaking countries.
Alexander Kleger's team at the Institute of Molecular Oncology and Stem Cell Biology was one of the first to succeed in cultivating exocrine pancreatic organoids, i.e. cell structures consisting exclusively of cells from the pancreatic duct or glandular tissue, from human pluripotent stem cells. These are used to better observe the development of precancerous stages and to create customised model tumours for further research. As pancreatic carcinoma is one of the most aggressive forms of tumour, this experimental work is also of great clinical relevance.